Abstract
Introduction: Refractory and relapsed AML (R/R AML) is difficult to treat with median overall survival of 6.5-39 months in patients undergoing allogeneic hematopoietic cell transplantation (alloHCT), and 1.5-11.9 months in patients not eligible for alloHCT. Venetoclax combined with fludarabine, cytarabine, and idarubicin (FLAVIDA) induces a high response rate in R/R AML patients. However, long-term outcome of this regimen has not been compared to FLA-IDA chemotherapy only.
Objectives: To compare FLAVIDA with FLA-IDA as salvage chemotherapy in R/R AML and assess MRD response and overall survival (OS).
Methods: This retrospective single center cohort study included patients with R/R AML treated with FLAVIDA or FLA-IDA. Venetoclax was dosed 100mg/day orally (days 1-7) due to co-medication with posaconazole. Eighty-one patients that were treated with FLA-IDA between 2000 and 2018 and fulfilled the selection criteria of the FLAVIDA patients served as control. Measurable residual disease (MRD) was assessed by NGS with a cutoff of 0.01% or multicolor flow cytometry with a cutoff of 0.1%. The overall response rate was defined by complete remission (CR) + CR with incomplete hematologic recovery (CRi) + morphologic leukemia-free state (MLFS). This study was approved by the local Ethics Review Committee in accordance with the Declaration of Helsinki. and is registered with ClinicalTrials.gov, NCT03662724. The data cut-off for this analysis was December 31, 2021.
Results: Thirty-seven and 81 patients, who received one course of FLAVIDA and FLA-IDA, respectively, were included in the analysis. Baseline characteristics were balanced between FLAVIDA and FLA-IDA treated patients: median age 54 vs. 52 years; de novo AML 70% vs. 77%; 2017 ELN adverse risk 33% vs. 25%; relapsed AML 51% vs. 42%; prior alloHCT 22% vs. 28%. FLAVIDA and FLA-IDA treated patients received a median of one (range 1-5) prior lines of therapy.
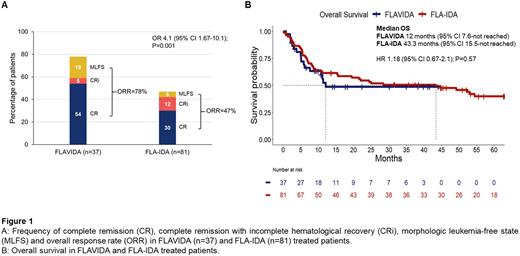
The ORR was 78% (n=29/37) in the FLAVIDA compared to 47% (n=38/81) in the FLA-IDA group (P=0.001) (Figure 1A). The CR/CRi rate was 59% and 30% in FLAVIDA and FLA-IDA patients, respectively (P=0.003). MRD negative response was achieved in a similar proportion of patients treated with the two regimens (50% and 57%; P=0.65).
No differences in neutrophil and platelet recovery times were observed in the FLAVIDA compared to the FLA-IDA group. Most commonly observed treatment related toxicities of any grade were hematological adverse events (AEs) being reported in all FLAVIDA treated patients. Non-hematological AEs of all grades included bacteremia, sepsis, and fungal pneumonia occurring in 27%, 11%, and 11%, respectively.
Eighty-one and 79% of patients proceeded to alloHCT or donor lymphocyte infusion (DLI) after FLAVIDA and FLA-IDA, respectively.
Median follow up was 22.4 and 62.9 months in FLAVIDA and FLA-IDA cohorts. Despite a higher ORR in FLAVIDA patients, OS was similar between FLAVIDA and FLA-IDA-treated patients (HR 1.18; P=0.57) (Figure 1B). In the 26 responding FLAVIDA patients with available MRD data, survival was significantly longer in MRD negative patients (HR 0.1, 95%CI 0.01-0.82; P=0.009) while MRD was not prognostic for OS in responding FLA-IDA patients with available samples (n=23; HR 0.58, 95%CI 0.17-1.9; P=0.36). Subgroup analyses revealed that the only group with different EFS and OS after FLAVIDA or FLA-IDA was the non-responding patient group, in which FLA-IDA treated patients had improved EFS and OS after additional salvage treatment. Median OS from the time of non-response was significantly longer in non-responding FLA-IDA compared to non-responding FLAVIDA patients (HR 0.31, 95%CI 0.12-0.8; P=0.01), suggesting that non-responding FLA-IDA patients could be salvaged more successfully.
Conclusions: Short-term venetoclax in combination with FLA-IDA represents an effective intensive treatment regimen in R/R AML. ORR was significantly higher in FLAVIDA compared to FLA-IDA treated patients. However, OS was comparable among patients treated with FLAVIDA or FLA-IDA. MRD negative response was associated with excellent OS in FLAVIDA treated patients.
Disclosures
Shahswar:Jazz Pharmaceuticals: Honoraria; AbbVie: Honoraria. Koenecke:Novartis: Membership on an entity's Board of Directors or advisory committees. Thol:Takeda: Membership on an entity's Board of Directors or advisory committees; Novartis: Membership on an entity's Board of Directors or advisory committees; AbbVie: Membership on an entity's Board of Directors or advisory committees; BMS: Membership on an entity's Board of Directors or advisory committees. Heuser:Jazz Pharmaceuticals: Consultancy, Honoraria, Research Funding; Janssen: Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Takeda: Honoraria; Agios: Consultancy, Research Funding; BMS: Consultancy; Daiichi Sankyo: Consultancy, Research Funding; Glycostem: Consultancy, Research Funding; Kura Oncology: Consultancy; Pfizer: Consultancy, Research Funding; PinotBio: Consultancy, Research Funding; Roche: Consultancy, Research Funding; Tolremo: Consultancy; Abbvie: Consultancy, Honoraria, Research Funding; Eurocept: Honoraria; Astellas: Research Funding; Bayer Pharma AG: Research Funding; BergenBio: Research Funding; Loxo Oncology: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal